Precision detection of foodborne illness pathogens
Enhancing food safety with advanced NGS and dPCR methods
Battling foodborne illness: Advanced technologies for pathogen detection
Foodborne pathogens pose a significant threat to public health, contaminating the food supply and causing severe illness. The complexity and adaptability of these microorganisms require sophisticated detection methods. Our next-generation sequencing (NGS) and digital PCR (dPCR) products offer the precision and accuracy needed to safeguard food safety, ensuring that even the most elusive pathogens are confidently identified and quantified.
The biology of foodborne pathogens: Adaptations, toxins and their impact on food safety
Meet the microbes: Understanding the pathogens behind foodborne illness
Scientific challenges in detecting foodborne pathogens: The need for advanced methods
Choosing the right tool for studying foodborne illness pathogens: NGS and dPCR

Tailored foodborne pathogen detection: QIAseq xHYB Microbial Panels
Unlock the full potential of your pathogen research with QIAseq xHYB Microbial Panels. Whether you need a fully customized solution targeting your specific organisms of interest or prefer the ease and efficiency of our expertly designed catalog panels, we've got you covered. Our user-friendly custom design tool allows you to create panels that provide comprehensive coverage and deep insights, empowering you to detect and characterize even the most elusive pathogens with precision and confidence.
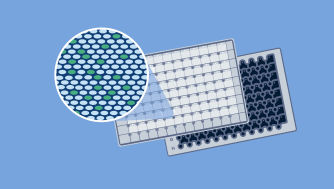
Precision and sensitivity combined: dPCR assays targeting foodborne illness pathogens
Our collection of dPCR Microbial DNA Detection Assays offers a powerful toolkit for precise and reliable detection of foodborne pathogens. These assays are designed to seamlessly integrate with the QIAcuity Digital PCR System, supporting flexible multiplexing for analyzing multiple targets in a single reaction. Many of our predesigned assays have undergone rigorous dPCR wet-lab testing, ensuring the highest standards of performance and reliability for your food safety research.
Organism Type
Organism Type | Species | NCBI Taxonomy ID | Assay Catalog # |
|---|---|---|---|
| Bacteria | Aeromonas caviae | 648 | Design a Custom Assay |
| Bacteria | Aeromonas hydrophila | 644 | DMA00020 |
| Bacteria | Aeromonas sobria | 646 | Design a Custom Assay |
| Bacteria | Aliarcobacter butzleri | 28197 | DMA00033 |
| Bacteria | Bacillus cereus | 1396 | DMA00041 |
| Bacteria | Campylobacter jejuni | 197 | DMA00084 |
| Bacteria | Clostridium perfringens | 1502 | DMA00109 |
| Bacteria | Corynebacterium ulcerans | 65058 | DMA00794 |
| Bacteria | Coxiella burnetii | 777 | DMA00123 |
| Bacteria | Escherichia coli | 562 | DMA00140 |
| Bacteria | Escherichia coli (eae) | 562 | DMA00698 |
| Bacteria | Escherichia coli (rfbE) | 562 | DMA00699 |
| Bacteria | Escherichia coli (stx1) | 562 | DMA00696 |
| Bacteria | Escherichia coli (stx2) | 562 | DMA00697 |
| Bacteria | Listeria monocytogenes | 1639 | DMA00199 |
| Bacteria | Plesiomonas shigelloides | 703 | DMA00257 |
| Bacteria | Salmonella | 590 | DMA00704 |
| Bacteria | Salmonella enterica | 28901 | DMA00291 |
| Bacteria | Salmonella enterica subsp. enterica | 59201 | DMA00360 |
| Bacteria | Shigella dysenteriae | 622 | DMA00295 |
| Bacteria | Shigella sonnei | 624 | DMA00361 |
| Bacteria | Staphylococcus aureus | 1280 | DMA00302 |
| Bacteria | Vibrio cholerae | 666 | DMA00340 |
| Bacteria | Vibrio parahaemolyticus | 670 | DMA00341 |
| Bacteria | Vibrio vulnificus | 672 | DMA00342 |
| Bacteria | Yersinia enterocolitica | 630 | DMA00344 |
| Bacteria | Yersinia pseudotuberculosis | 633 | Design a Custom Assay |
| Virulence Genes | Enterotoxigenic Ecoli, LT | DMA00612 | |
| Virulence Genes | estA1 | DMA00613 | |
| Viruses | Enterovirus | 12059 | DMA00487 |
| Viruses | Hepatitis E virus | 291484 | DMA00750 |
| Viruses | Human hepatitis A virus | 208726 | DMA00807 |
| Viruses | Human rotavirus A | 10941 | DMA00488 |
| Viruses | Norovirus GI | 122928 | DMA00472 |
| Viruses | Norovirus GII | 122929 | DMA00473 |
Items per page:
100
1 – 35 of 35